Across social media platforms, the hashtag “#cortisolface” has gained traction, with many users claiming that facial swelling and puffiness are due to elevated cortisol levels. Influencers often start their videos with statements like, “You’re not ugly, you just have cortisol face,” and promote various remedies and lifestyle changes as solutions. However, experts warn that although high cortisol can contribute to these symptoms, it is not the sole cause of facial puffiness.
Before blindly believing social media trends, it’s crucial to explore the underlying causes, which might include medications, health conditions or lifestyle factors. Addressing high cortisol levels requires a different approach than what many of these social media influencers suggest.
Dr. Maria Olenick, associate professor at Texas A&M University School of Nursing, offers valuable insights into the concept of “cortisol face,” its effects on the body, and methods for lowering cortisol levels.
What Is ‘Cortisol Face’?
Although high cortisol levels are a factor in some cases of facial swelling and puffiness, the symptom is not as common as social media is making it out to be. In some cases, it’s not cortisol but the foods you eat. For example, eating a meal or snack that’s high in sodium can make you feel bloated because the salt can cause you to retain fluid and look a little puffier than normal.
“Some of the more severe things like moon face and other symptoms are what you might consider a serious issue when a person should really go and see their health care provider, because that would require some medical diagnosis,” Olenick said.
Moon face—or moon facies, in medical terminology—describes an increase of facial swelling due to high cortisol levels. This is a more serious condition that doesn’t just appear or disappear from one day to the next.
How Does Cortisol Affect The Body?
Cortisol is referred to as the body’s “built-in alarm system” because it plays a crucial role in the body’s response to stress, metabolism, immune activity and maintaining homeostasis. The amount of cortisol produced will differ from day to day due to different mental and physical stressors.
“Among healthy individuals, cortisol follows a diurnal pattern in which levels are higher upon waking, increase significantly over about 30 minutes, and steadily decrease from the peak throughout the rest of the day, reaching the nadir in the middle of the night,” said Olenick, whose research focuses on effective stress management techniques and therapies for veterans dealing with post-traumatic stress disorder (PTSD).
Hormones act as chemical messengers working through your bloodstream to regulate various bodily functions. Cortisol, often called the stress hormone, utilizes receptors that receive and use the hormone in different ways by communicating with your brain to control your mood, motivation and fear.
Different ways cortisol reacts and adapts to cope in a stress state include:
- Regulating blood pressure
- Regulating metabolism
- Regulating blood sugar
- Managing how your body uses carbohydrates, fats and proteins
- Suppressing inflammation
- Helping control your sleep/wake cycle
- Aiding in forming memories
Cortisol secretion is regulated by a hormonal axis through a feedback loop that involves your hypothalamus, pituitary gland, adrenal glands and certain hormones known as the hypothalamic-pituitary-adrenal (HPA) axis. The hypothalamus and pituitary gland in your brain monitor your blood’s cortisol levels before signaling the adrenal glands, which sit on top of each kidney. When a change in cortisol levels is detected, your adrenal glands react to these signals by adjusting the amount of cortisol needed to be released.
The feedback system starts when the hypothalamus detects stress and releases corticotrophin-releasing hormone (CRH) accordingly. This hormone travels into the pituitary gland, signaling it to secrete adrenocorticotropic hormone (ACTH). ACTH will then make its way to the adrenal glands, stimulating them to produce cortisol. Once produced, cortisol is released into the bloodstream, where it helps regulate various functions including stress response, metabolism and immune activity. The HPA axis feedback loop is completed when cortisol levels rise and signal the hypothalamus to reduce CRH production, which maintains an effective secretion loop.
What Causes High Cortisol Levels?
Cortisol is increased at times of stress for your body, but our bodies aren’t designed to handle long-term stress. When there’s too much cortisol or an excess amount of cortisol produced, it can cause major changes in your body’s everyday functions.
Chronic emotional or physical distress can lead to sustained high levels of cortisol as part of the body’s stress response system. Stress activates signals that prompt the adrenal glands to release hormones like adrenaline and cortisol, leading to an increased heart rate and heightened energy for the fight-or-flight response.
Cortisol temporarily suppresses non-essential functions such as digestion, reproduction and inflammation in the short term to prepare for danger. However, if stress is constant, this response can remain active, which can negatively impact many bodily functions such as sleep, weight management, memory, focus and mental health. Chronic stress can also increase the risk of anxiety, depression, digestive issues, headaches, muscle tension, pain and high blood pressure.
However, stress is not the only culprit for excess cortisol levels. It could indicate serious underlying health issues.
“You need to make sure that if you are having issues with cortisol levels that you don’t really have a tumor or something more serious. If you feel like you are having symptoms and they’re not resolved by implementing lifestyle changes, make sure you see a health care provider, because that could be something very different and it might need significant medical care,” Olenick said.
Cushing Syndrome
Cushing syndrome, also known as hypercortisolism, is characterized by excessive levels of cortisol in the body. Prolonged use of corticosteroid medications can result in exogenous Cushing syndrome, where the excess cortisol originates from external sources rather than the body’s own production. One common cause of high cortisol levels is the use of glucocorticoid medications, such as prednisone, which are prescribed for inflammatory conditions like asthma, rheumatoid arthritis and lupus.
“Sometimes people are on steroids such as prednisone for a different condition. When you’re taking steroids, if you start to show signs of serious cortisol issues, talk to your provider,” Olenick said.
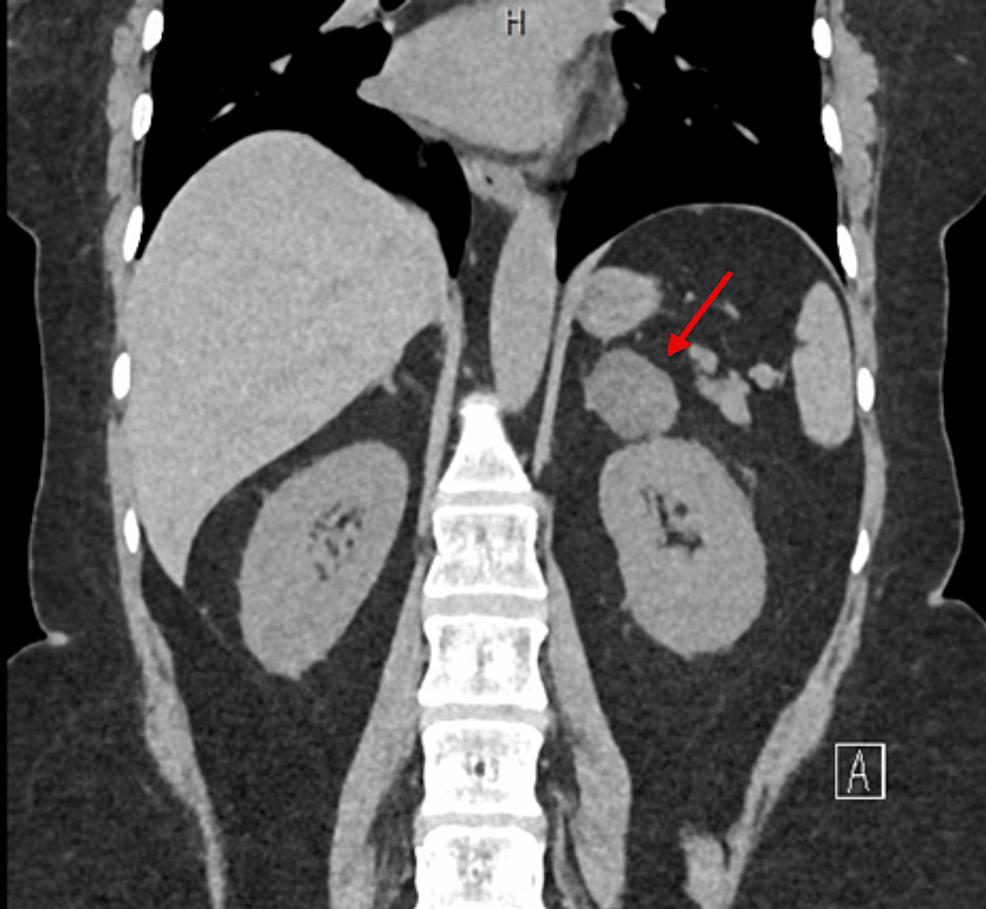
Another significant cause of Cushing syndrome is pituitary tumors that secrete excessive amounts of ACTH, which overstimulates the adrenal glands to produce more cortisol. This form of Cushing syndrome, known as Cushing disease, is attributed to benign pituitary adenomas and accounts for a large proportion of cases in both adults and children. Effective management of Cushing syndrome involves addressing the underlying cause, which may include surgical removal of tumors or adjusting medication regimens to reduce cortisol levels and mitigate associated health challenges.
Adrenal gland tumors can also contribute to high cortisol levels. These tumors may be benign or malignant, leading to similar symptoms as those caused by pituitary tumors. Tumors affecting either the pituitary gland or adrenal glands can lead to elevated cortisol levels, but most of these tumors are noncancerous and may be manageable with proper medical care.
Understanding the underlying causes of high cortisol levels is crucial for appropriate diagnosis and treatment, as the medical implications of these conditions extend beyond the portrayals seen in popular media.
What Are Common Symptoms Of High Cortisol Levels?
Having the right cortisol balance is essential for your health, and producing too much or too little can cause health problems, including:
- Puffiness or weight gain in the face
- Weight gain in the midsection or abdomen
- Excess fat behind the neck, above the back
- Memory and concentration problems, or brain fog
- Trouble sleeping, or insomnia
- Severe fatigue
- High blood pressure
- Psychiatric disturbances
Symptoms may vary, so the only real way to validate if your cortisol levels are higher than normal is to get them checked, either with blood, urine or saliva tests. When Olenick evaluates cortisol levels in veterans for PTSD research, her preferred method is to collect samples of saliva. A saliva test can be conducted at home, but it’s most effective when collected at different times throughout the day.
How Can Someone Lower Their Cortisol Levels?
Maintaining a healthy diet, sticking to a regular sleep schedule and incorporating regular, moderate exercise can all help lower cortisol. It’s also important to manage stress effectively; this can involve finding healthy ways to cope with stress, such as talking to someone you trust or allowing yourself time to relax and unwind. Self-care is crucial—taking breaks and engaging in activities that rejuvenate you is not a waste of time but a necessary part of maintaining balance.
Avoid extreme measures like severe caloric restriction or high-intensity workouts, which can increase cortisol levels due to the stress they place on the body. Instead, go for low-intensity exercises like walking. Additionally, Olenick says natural remedies and supplements, such as apple cider vinegar and vitamins, may support cortisol management, but it’s wise to monitor their effects and consult with a health care provider if needed. Ultimately, finding a balance between self-care, stress management and maintaining a healthy lifestyle is key to controlling cortisol levels effectively.
“There are a lot of things you can do to regulate your cortisol, like eating well, sleeping well and lowering our stress. Basically, things to take care of ourselves,” Olenick said.
Olenick says social media platforms are great attention grabbers, but it’s important to take health trends with a grain of salt and pay attention to your body’s needs. If you relate to any of the symptoms and feel concerned about your cortisol levels, notify your health care provider and seek medical attention.
This article by Teresa Saenz originally appeared on Vital Record.
Filed under: Cushing's, symptoms | Tagged: cortisol, Cortisol Face, facial rounding, moon face, moonface, stress | Leave a comment »