Abstract
Introduction
Hypertension is one of the most common clinical features of patients with overt and subclinical hypercortisolism. Although previous studies have shown the coexistence of autonomous cortisol and aldosterone secretion, it is unclear whether aldosterone plays a role in hypertension among patients with hypercortisolism. Therefore, we examined the associations of plasma aldosterone concentrations (PACs) with hypertension among patients with overt and subclinical hypercortisolism.
Methods
This single-center retrospective cohort study included patients with adrenal tumor and serum cortisol levels after 1-mg dexamethasone suppression test >1.8 µg/dL (50 nmol/L). Using multivariable regression models adjusting for baseline characteristics, we investigated the association of PACs with systolic blood pressure and postoperative improvement of hypertension after the adrenalectomy.
Results
Among 89 patients enrolled in this study (median age, 51 years), 21 showed clinical signs of Cushing syndrome (overt hypercortisolism) and 68 did not show clinical presentations (subclinical hypercortisolism). We found that higher PACs were significantly associated with elevated systolic blood pressure among patients with subclinical hypercortisolism (adjusted difference [95% CI] = +0.59 [0.19-0.99], P = 0.008) but not among those with overt hypercortisolism. Among 33 patients with subclinical hypercortisolism and hypertension who underwent adrenalectomy, the postoperative improvement of hypertension was significantly associated with higher PACs at baseline (adjusted risk difference [95% CI] = +1.45% [0.35-2.55], P = 0.01).
Conclusion
These findings indicate that aldosterone may contribute to hypertension among patients with subclinical hypercortisolism. Further multi-institutional and population-based studies are required to validate our findings and examine the clinical effectiveness of the intervention targeting aldosterone for such patients.
Cortisol production in the adrenal gland is regulated by the hypothalamus-pituitary-adrenal (HPA) axis. Subclinical hypercortisolism is a status characterized by the alteration of HPA axis secretion without typical signs or symptoms of overt hypercortisolism (eg, moon face, truncal obesity, easy bruising, thin extremities, proximal myopathy, cutaneous purple striae) [1, 2]. Although overt hypercortisolism can be detected by its clinical presentations or severe complications, it is sometimes challenging for clinicians to appropriately diagnose subclinical hypercortisolism because of the absence of such clinical presentations [2]. The 1-mg overnight dexamethasone suppression test (1-mg DST) measures the response of the adrenal glands to ACTH through the HPA axis and therefore has been widely used for screening and diagnosis of subclinical hypercortisolism [1, 3]. The European Society of Endocrinology Guideline has defined a partial suppression of the HPA axis (ie, serum cortisol levels after 1-mg DST [F-DST] > 1.8 µg/dL [50 nmol/L]) without clinical signs of overt cortisol hypersecretion as “possible autonomous cortisol secretion” and recommended screening these patients for metabolic disorders including hypertension and type 2 diabetes mellitus to offer appropriate treatment of these comorbidities [4].
Hypertension is one of the most common and distinguishing clinical features in patients with subclinical hypercortisolism [2] as well as overt hypercortisolism [5]. Although hypertension can be triggered by excess cortisol levels [5, 6], it is still unclear whether even slightly elevated cortisol levels among individuals with subclinical hypercortisolism contribute to the occurrence of hypertension. This raises another potential mechanism to cause hypertension such as the coexistence of hyperaldosteronism (ie, excess aldosterone that is an essential steroid hormone for sodium reabsorption, water retention, and blood pressure control) [7]. Previous studies have reported that 10% to 20% of primary aldosteronism is accompanied by cortisol-producing adenoma [8-10], and autonomous cortisol secretion was decreased after the resection of the aldosterone-producing adenoma (a subtype of primary aldosteronism) [11]. Furthermore, a previous mass spectrometry-based analysis revealed that cortisol secretion was frequently found in patients with primary aldosteronism [12]. Although these studies have examined cortisol biosynthesis in primary aldosteronism [13], evidence about whether aldosterone plays a role in the occurrence of hypertension among people with subclinical hypercortisolism is limited.
To address this knowledge gap, we performed a cohort study examining the association between aldosterone and hypertension among patients with adrenal tumor and F-DST >1.8 µg/dL, stratified by whether patients had clinical signs of Cushing syndrome or not. We first analyzed the cross-sectional association between aldosterone and blood pressure at baseline. Then, we analyzed the longitudinal association between aldosterone at baseline and the improvement rate of hypertension after the adrenalectomy. Last, to further clarify the role of aldosterone in the regulation of blood pressure in subclinical hypercortisolism, we described the difference in aldosterone response to ACTH after the adrenalectomy according to the postoperative improvement of hypertension.
Materials and Methods
Data Sources and Study Participants
A retrospective cohort study was designed to assess the clinical characteristics (focusing on aldosterone) among patients with hypercortisolism at the Yokohama Rosai Hospital from 2008 to 2017. We enrolled 89 patients with adrenal tumor and F-DST > 1.8 µg/dL (50 nmol/L) [3, 4, 14]. We then categorized them into 2 groups: (1) overt hypercortisolism (F-DST > 5.0 µg/dL [138 nmol/L]) and having clinical signs of Cushing syndrome (moon face, central obesity, dorsocervical fat pad [buffalo hump], purple striae, thin skin, easy bruising, and proximal myopathy] [15]) and (2) subclinical hypercortisolism (not having such clinical signs). All patients with overt hypercortisolism in this study showed F-DST > 5.0 µg/dL (138 nmol/L). The study was approved by the research ethics committee of the Yokohama Rosai Hospital, and all participants provided written informed consent.
Measurements
Demographic characteristics were self-reported, and body mass index (BMI) was calculated using measured weight and height. Systolic blood pressure was measured in the sitting position using a standard upper arm blood pressure monitor after a 5-minute rest in a quiet place [16]. The mean of 2 measurements was recorded. If the measurement was done only once on a given occasion, the level obtained was recorded. When the patients were already taking antihypertensives at enrollment, they were asked to report their blood pressure levels at the diagnosis of hypertension (ie, systolic blood pressure before starting antihypertensives). Blood samples were collected at 8:00 AM after the patient had rested in the supine position for 30 minutes. We measured F (µg/dL, × 27.6 for nmol/L) and ACTH (pg/mL, × 0.220 for pmol/L) using chemiluminescent enzyme immunoassay and electrochemiluminescent immunoassay, respectively. Plasma aldosterone concentrations (PACs; ng/dL, × 27.7 for pmol/L) and plasma renin activities (PRAs; ng/mL/h) were measured using radioimmunoassay. Any antihypertensive drugs were replaced with calcium channel antagonists (including dihydropyridine calcium channel antagonists) and/or α blocker several weeks before the measurement of PACs and PRAs according to the clinical guideline of the Japan Endocrine Society [17]. We also measured urine aldosterone (µg/day × 2.77 for nmol/d) and urine cortisol (µg/day, × 2.76 for nmol/d) using radioimmunoassay. The tumor size was estimated using contrast-enhanced thin-section computed tomography scans of the adrenal glands.
To evaluate whether the patients had autonomous cortisol secretion, we performed 1-mg DST, in which dexamethasone (1 mg) was administered at 11:00 PM, and blood samples were drawn at 8:00 AM the following morning. F and ACTH were measured in 1-mg DST.
The total or partial adrenalectomy was performed in all cases with overt hypercortisolism. For patients with subclinical hypercortisolism, the adrenalectomy was recommended to those who showed F-DST > 5.0 µg/dL (138 nmol/L) accompanying metabolic disorders [3]. It was also recommended to those who were expected to improve their clinical symptoms and/or metabolic disorders by the tumor resection, which included patients with hypertension possibly resulting from autonomous aldosterone secretion as well as autonomous cortisol secretion from the adrenal gland. The adrenalectomy was conducted when patients agreed with the treatment plan through informed consent. To evaluate whether patients had autonomous aldosterone secretion, we used the screening criterion of primary aldosteronism (ie, PAC/PRA ratio; aldosterone-to-renin ratio [ARR] > 20), followed by the confirmatory tests of primary aldosteronism that included the saline infusion test, captopril challenge, and/or furosemide stimulation test [17].
For patients who were considered to receive a benefit by the adrenalectomy and who agreed with the examination, we performed the segment-selective adrenal venous sampling to assess the laterality of hyperaldosteronism [18-20]. First, blood samples were collected from the bilateral central adrenal veins before ACTH stimulation. Then, we collected samples from the superior, lateral, and inferior tributaries of the right central adrenal vein and the superior and lateral tributaries of the left central adrenal vein after ACTH stimulation. Aldosterone excess (ie, hyperaldosteronism) was considered when the effluent aldosterone concentrations were > 250 ng/dL before ACTH stimulation and 1400 ng/dL after ACTH stimulation, respectively [18-20]. We used the absolute value instead of the lateralization index because individuals included in our study had elevated cortisol concentrations given the inclusion criteria (ie, F-DST >1.8 µg/dL [50 nmol/L]). For 9 patients with subclinical hypercortisolism who showed bilateral adrenal nodules, the side of adrenalectomy was determined by the nodule size and the results of adrenal venous sampling (ie, laterality of hyperaldosteronism). The adrenalectomy was conducted when patients agreed with the treatment plan through informed consent. Immunohistochemical evaluation of aldosterone synthase cytochrome P450 (CYP11B2) was conducted for some resected nodules.
To evaluate the postoperative cortisol responsiveness to ACTH, we performed an ACTH stimulation test a year after the adrenalectomy, in which blood samples were collected and PAC and F were measured 30 and 60 minutes after ACTH administration. Postoperative improvement of hypertension was defined as blood pressure <140/90 mmHg without antihypertensives or the reduction of the number of antihypertensives to maintain blood pressure <140/90 mmHg after the adrenalectomy.
Statistical Analyses
We describe the demographic characteristics and endocrine parameters at baseline comparing patients with overt hypercortisolism and those with subclinical hypercortisolism using the Fisher exact test for categorical variables and Mann-Whitney U test for continuous variables. Second, for each group, we investigated the association between the baseline characteristics and systolic blood pressure using ordinary least-squares regression models. The model included age, sex, BMI, serum potassium levels, estimated glomerular filtration rate, tumor size, and F and PAC at 8:00 AM. Third, we estimated the risk difference and 95% CI of the improvement rate of hypertension after the adrenalectomy according to these baseline characteristics (including systolic blood pressure) using a modified least-squares regression model with a Huber-White robust standard error [21]. Last, to evaluate whether the improvement of hypertension is related to postoperative cortisol and aldosterone secretion, we compared PAC and F responsiveness to ACTH from peripheral blood samples between patients who improved hypertension and those who did not using the Mann-Whitney U test. The longitudinal and postoperative analyses were performed among patients with subclinical hypercortisolism because only 2 cases with overt hypercortisolism failed to show the improvement of hypertension after the adrenalectomy.
To assess the robustness of our findings, we conducted the following 2 sensitivity analyses. First, we replaced F at 8:00 AM with F after DST in our regression models. Second, we estimated the risk difference of the improvement rate of hypertension after the adrenalectomy according to the postoperative F and PAC levels after ACTH stimulation, adjusting for the baseline characteristics included in our main model.
We also conducted several additional analyses. First, to investigate the relationship of change in PAC after adrenalectomy with the improvement rate of hypertension, we included decrease in PAC between before and after adrenalectomy instead of PAC at baseline in the model. Second, to assess the relationship between aldosterone and hypertension among patients with subclinical hypercortisolism without primary aldosteronism, we reran the analyses excluding patients who met the diagnostic criteria of primary aldosteronism. Third, to understand the overall association, we reran the analyses using all samples as a single group to assess the relationship among people with overall (ie, overt and subclinical) hypercortisolism. Last, we compared PAC and F responsiveness with ACTH during adrenal venous sampling between patients with and without postoperative improvement of hypertension. All statistical analyses were performed using Stata, version 15.
Results
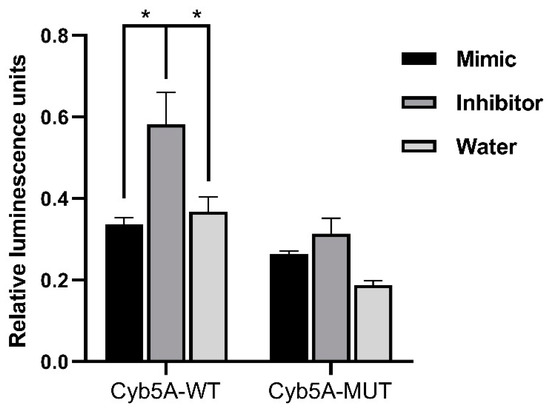
Among the 89 enrolled patients, 21 showed clinical signs of overt Cushing syndrome and 68 did not. The flow of the study population is shown in Fig. 1. Among 21 patients with overt hypercortisolism, 19 patients had hypertension. All patients underwent adrenalectomy, and 16 patients showed improved hypertension levels after the surgery (1 patient was referred to another hospital; therefore, no information is available). Among 68 patients with subclinical hypercortisolism, 63 had hypertension. After the evaluation of autonomous aldosterone secretion as well as autonomous cortisol secretion, of 33 patients who underwent adrenalectomy, 23 (70%) showed improved hypertension levels after the adrenalectomy (10 patients in the surgery group decided not to undergo adrenalectomy). Patients with subclinical hypercortisolism who underwent adrenalectomy showed lower PRA and higher ARR than those without adrenalectomy (Supplementary Table S1) [22].
Figure 1.
![Enrollment and follow-up of the study population after the adrenalectomy. aThe prevalence of patients with overt hypercortisolism and hypertension among this study population may be higher than in the general population and therefore needs to be carefully interpreted given that the study institute is one of the largest centers for adrenal diseases in Japan. bAll patients in this category showed autonomous cortisol secretion (ie, serum cortisol levels >5.0 µg/dL [138 nmol/L] after a 1-mg dexamethasone suppression test). cOne case underwent adrenalectomy at another hospital and therefore no information was available after the adrenalectomy. dThe adrenalectomy was performed for 33 patients who were expected to improve their clinical symptoms and/or metabolic disorders, including hypertension. This assessment was mainly based on autonomous cortisol secretion evaluated by a 1-mg dexamethasone suppression test, complicated metabolic disorders, and autonomous aldosterone secretion evaluated by adrenal venous sampling for patients who were positive for the screening and confirmatory tests of primary aldosteronism. Details in the assessment can be found in the Methods section or elsewhere [18-20].](https://oup.silverchair-cdn.com/oup/backfile/Content_public/Journal/jes/7/1/10.1210_jendso_bvac167/2/m_bvac167f1.jpeg?Expires=1673226229&Signature=lH6Fo2svnZ4zLJ1vgDEWEShEHMnJYbw7JNP1Va6L~hR1SEu38yoBriwSZN9YHqMv3KcleFNJHIJun5Q0YYsBF9KclE-FpKJ0hmyzTCE6ZPxtRFpYNYDFSPY~4HTccGaYS6NvslM7g4mleOc1ZalfFRPRAzNZAeIvsLeaKXeF4pXP5dqL0W1jT-SgLyVkPbVhteCGMSm4fLytXM85yaB0AhExA3WwQuihmQU1sYbI0BeOE5tneusxGAFbxZDx2CbCT1UuYvaYHNAYQ6Q7NHMF2cpE0fW9HSkUpejOb5zgycvPAFaPiWmDZxoHDDhCIVzuUFpr7ngYe7MoS2O-QKd6tA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
Enrollment and follow-up of the study population after the adrenalectomy. aThe prevalence of patients with overt hypercortisolism and hypertension among this study population may be higher than in the general population and therefore needs to be carefully interpreted given that the study institute is one of the largest centers for adrenal diseases in Japan. bAll patients in this category showed autonomous cortisol secretion (ie, serum cortisol levels >5.0 µg/dL [138 nmol/L] after a 1-mg dexamethasone suppression test). cOne case underwent adrenalectomy at another hospital and therefore no information was available after the adrenalectomy. dThe adrenalectomy was performed for 33 patients who were expected to improve their clinical symptoms and/or metabolic disorders, including hypertension. This assessment was mainly based on autonomous cortisol secretion evaluated by a 1-mg dexamethasone suppression test, complicated metabolic disorders, and autonomous aldosterone secretion evaluated by adrenal venous sampling for patients who were positive for the screening and confirmatory tests of primary aldosteronism. Details in the assessment can be found in the Methods section or elsewhere [18-20].
Demographic Characteristics and Endocrine Parameters Among Patients With Overt and Subclinical Hypercortisolism
The median age (interquartile range) was 51 years (46, 62 years), and 72% were female. Patients with overt hypercortisolism were relatively younger and showed a higher estimated glomerular filtration rate and larger tumor size compared with patients with subclinical hypercortisolism (Table 1). Other demographic characteristics were similar between these groups. Patients with overt hypercortisolism showed higher F with undetected low ACTH, higher F after DST, and higher urine cortisol levels compared with those with subclinical hypercortisolism who instead showed higher PAC and ARR. Among patients with subclinical hypercortisolism, 9/68 (13.2%) showed undetectable ACTH levels and 25/68 (36%) were positive for PA screening criterion (ie, ARR > 20) followed by at least 1 positive confirmatory test. Based on the results of adrenal venous sampling of these cases, 9 showed aldosterone excess in the right nodules, 6 showed aldosterone excess in the left nodules, and 7 showed aldosterone excess on both sides, respectively (3 cases did not show aldosterone excess on both sides). Immunohistochemical evaluation of CYP11B2 was examined for 6 resected adrenal glands, and all of them showed positive expression.
| Patients’ characteristicsa |
Patients with overt hypercortisolism (N = 21) |
Patients with subclinical hypercortisolism (N = 68) |
P |
| Age, y |
46 [38-52] |
54 [47-63] |
0.002 |
| Female, n (%) |
18 (85.7) |
46 (67.7) |
0.11 |
| Body mass index, kg/m2 |
23.4 [20.6-26.2] |
23.1 [21.7-25.1] |
0.94 |
| Systolic blood pressure, mm Hg |
156 [140-182] |
162 [151-191] |
0.29 |
| Diastolic blood pressure, mm Hg |
98 [92-110] |
100 [90-110] |
0.73 |
| Serum potassium, mEq/Lb |
3.9 [3.5-4.0] |
3.8 [3.6-4.0] |
0.98 |
| eGFR, mL/min/1.73 m2 |
86.7 [77.3-123.0] |
82.1 [69.8-87.7] |
0.02 |
| Tumor size by CT scan, mm |
28 [25-30] |
22 [17-26] |
0.001 |
| ACTH, 8:00 AM |
− c |
6.6 [2.4-11.8] |
— |
| F, 8:00 AM |
16.6 [12.5-18.8] |
9.5 [7.7-12.0] |
<0.001 |
| PRA, 8:00 AM |
0.7 [0.4-1.3] |
0.5 [0.2-1.0] |
0.10 |
| PAC, 8:00 AM |
8.3 [7.2-9.8] |
9.2 [7.2-16.2] |
0.09 |
| ARR, 8:00 AM |
10.0 [6.4-16.7] |
21.0 [9.8-46.5] |
0.02 |
| F after DST |
16.5 [14.4-18.7] |
5.1 [3.2-7.5] |
<0.001 |
| Urine cortisol |
220.0 [105.0-368.0] |
49.5 [37.4-78.5] |
<0.001 |
| Urine aldosterone |
5.7 [3.9-10.1] |
7.2 [4.8-13.1] |
0.16 |
Conversion to SI units: ACTH, pg/mL × 0.220 for pmol; F, µg/dL × 27.6 for nmol/L; PAC, ng/dL × 27.7 for pmol/L; urine aldosterone, μg/day × 2.77 for nmol/d; Urine cortisol, μg/day × 2.76 for nmol/d.
Abbreviations: ARR, aldosterone-to-renin ratio; CRH, corticotropin-releasing hormone; CT, thin-section computed tomography; DST, 1-mg dexamethasone suppression test; eGFR, estimated glomerular filtration rate; F, serum cortisol; PRA, plasma renin activity; PAC, plasma aldosterone concentration.
aData are presented as median (interquartile range) or count (proportions) unless otherwise indicated.
bSerum potassium levels were controlled using potassium supplement/tablets at enrollment.
cUndetected in all cases.
Association of Demographic Characteristics and Endocrine Parameters With Systolic Blood Pressure
Among patients with overt hypercortisolism, we did not find a significant association of demographic characteristics and endocrine parameters with systolic blood pressure (Table 2). However, among patients with subclinical hypercortisolism, we found that higher PACs at 8:00 AM were significantly associated with systolic blood pressure (adjusted coefficient [95% CI] = +0.59 [0.19-0.99], P = 0.008). The results did not change when we used F after DST instead of F at 8:00 AM (Supplementary Table S2) [22].
Table 2.
Cross-sectional association of demographic characteristics and endocrine parameters with systolic blood pressure among patients with overt and subclinical hypercortisolism
| Outcome |
Systolic blood pressure at baseline |
| Groups |
Patients with overt hypercortisolism |
Patients with subclinical hypercortisolism |
| Parameters |
Adjusted coefficient (95% CI) |
P |
Adjusted coefficient (95% CI) |
P |
| Age, y |
+1.73 (0.17-3.30) |
0.03 |
+0.49 (−0.13 to 1.10) |
0.12 |
| Female |
−7.48 (−76.75 to 61.79) |
0.81 |
+15.38 (−0.83 to 31.59) |
0.06 |
| Body mass index |
+5.47 (−2.4 to 13.33) |
0.15 |
+1.07 (−0.49 to 2.63) |
0.17 |
| Serum potassium |
+11.29 (−23.42 to 45.99) |
0.48 |
−9.61 (−26.38 to 7.15) |
0.26 |
| eGFR |
−0.12 (−1.00 to 0.77) |
0.77 |
−0.44 (−0.89 to 0.01) |
0.06 |
| Tumor size |
−2.39 (−6.92 to 2.14) |
0.26 |
+0.40 (−0.46 to 1.26) |
0.35 |
| F, 8:00 AMa,b |
+1.96 (−1.27 to 5.18) |
0.20 |
+1.26 (−1.00 to 3.52) |
0.27 |
| PAC, 8:00 AMa |
−2.86 (−7.38 to 1.66) |
0.18 |
+0.59 (0.19-0.99) |
0.008 |
Abbreviations: DST, 1-mg dexamethasone suppression test; eGFR, estimated glomerular filtration rate; F, serum cortisol; PRA, plasma renin activity; PAC, plasma aldosterone concentration.
aACTH and PRA were not included in the main model because they have strong correlation with F and PAC, respectively (ie, multicollinearity). The results did not change when additionally adjusting for ACTH and PRA.
bThe results did not change when we replaced F at 8:00 AM with F after DST (Supplementary Table S2).
Association of Demographic Characteristics and Endocrine Parameters With Hypertension Improvement After the Adrenalectomy Among Patients With Subclinical Hypercortisolism
Among 33 patients with subclinical hypercortisolism and hypertension who underwent the adrenalectomy, we found that age and higher PAC were significantly associated with a higher improvement rate of hypertension after the adrenalectomy (age, adjusted risk difference [95% CI] = +2.36% [1.08-3.64], P = 0.001; PAC, adjusted risk difference [95% CI] = +1.45% [0.35-2.55], P = 0.01; Table 3). The results did not change when we used F after DST instead of F at 8:00 AM (Supplementary Table S3) [22]. Patients with improved hypertension after the surgery showed significantly lower PACs 60 minutes after a postoperative ACTH stimulation test than those without the improvement of hypertension (P = 0.05), although F and PAC/F ratio were not significantly different between these 2 groups (Table 4). The association between lower PACs after postoperative ACTH stimulation and higher improvement rate of hypertension was also found in the multivariable regression analysis adjusting for baseline characteristics (adjusted risk difference [95% CI] = −1.08% [−1.92 to −0.25], P = 0.01; Supplementary Table S4) [22].
Table 3.
Longitudinal association of demographic characteristics and endocrine parameters with hypertension improvement after the adrenalectomy among patients with subclinical hypercortisolisma
| Outcome |
Hypertension improvement after the adrenalectomy |
| Parameters |
Adjusted risk difference (95% CI) |
P |
| Age |
+2.36% (1.08-3.64) |
0.001 |
| Sex (female) |
−11.32% (−61.37 to 38.73) |
0.64 |
| Body mass index |
−5.08% (−10.29 to 0.13) |
0.06 |
| Systolic blood pressure |
−0.67% (−1.77 to 0.43) |
0.22 |
| Serum potassium |
−0.06% (−31.84 to 31.71) |
1.00 |
| eGFR |
+0.53% (−0.36 to 1.42) |
0.23 |
| Tumor size |
+0.79% (−1.35 to 2.93) |
0.45 |
| F, 8:00 AMb,c |
−2.81% (−7.43 to 1.81) |
0.22 |
| PAC, 8:00 AMb |
+1.45% (0.35-2.55) |
0.01 |
Abbreviations: eGFR, estimated glomerular filtration rate; F, serum cortisol; PRA, plasma renin activity; PAC, plasma aldosterone concentration.
aAnalysis was not performed for patients with overt hypercortisolism because only 2/18 cases failed to show improved hypertension after the adrenalectomy.
bACTH and PRA were not included in the main model because they have strong correlation with F and PAC, respectively (ie, multicollinearity). The results did not change when additionally adjusting for ACTH and PRA.
cThe results did not change when we replaced F at 8:00 AM with F after DST (Supplementary Table S3).
Table 4.
Aldosterone and cortisol response to ACTH a year after the adrenalectomy according to hypertension improvement status among patients with subclinical hypercortisolisma
| Outcome: hypertension improvement status after the adrenalectomy |
Improvement (+) (N = 23) |
Improvement (−) (N = 10) |
|
| Parameters |
Median [IQR] |
Median [IQR] |
P |
| PAC 60 min after ACTH stimulation |
13.6 [10.0-16.7] |
15.5 [13.7-43.1] |
0.05b |
| F 60 min after ACTH stimulation |
16.9 [13.7-20.6] |
18.5 [13.5-24.7] |
0.61 |
| PAC/F ratio 60 min after ACTH stimulation |
0.70 [0.52-1.39] |
1.27 [0.50-5.44] |
0.26 |
Conversion to SI units: F, µg/dL × 27.6 for nmol/L; PAC, ng/dL × 27.7 for pmol/L.
Abbreviations: F, serum cortisol; PAC, plasma aldosterone concentration.
aAnalysis was not performed for patients with overt hypercortisolism because only 2/18 cases failed to show improved hypertension after the adrenalectomy.
bThe association was also observed after adjusting for baseline characteristics (eg, age, sex, body mass index, systolic blood pressure, serum potassium, estimated glomerular filtration rate, tumor size) and F 60 min after ACTH stimulation a year after the adrenalectomy (Supplementary Table S4).
Additional Analyses
Decreased PAC between before and after adrenalectomy was significantly associated with hypertension improvement (Supplementary Table S5) [22]. When we restricted samples to those without primary aldosteronism, PACs at baseline tended to be associated with systolic blood pressure but the 95% CI included the null (Supplementary Table S6) [22]. Decreased PAC after adrenalectomy was associated with hypertension improvement after the adrenalectomy, whereas PAC at baseline was not associated with that outcome (Supplementary Table S7) [22]. When we analyzed the entire sample (ie, both overt and subclinical hypercortisolism), PAC at baseline was associated with systolic blood pressure at baseline (Supplementary Table S8) [22] and hypertension improvement after the adrenalectomy (Supplementary Table S9) [22]. We also found the higher median value of PAC response to ACTH during adrenal venous sampling at the remained (ie, not resected by the adrenalectomy) side of adrenal gland among patients whose hypertension did not improve compared with those whose hypertension improved after the surgery, but the difference was not statistically significant (Supplementary Table S10) [22].
Discussion
In this retrospective cohort study, we found that higher aldosterone levels were associated with higher systolic blood pressure among patients with possible autonomous cortisol secretion and without clinical signs of overt Cushing syndrome (ie, subclinical hypercortisolism). In this group, higher aldosterone before the adrenalectomy was associated with the postoperative improvement of hypertension. Moreover, we found that patients with postoperative improvement of hypertension showed lower aldosterone response to ACTH after the adrenalectomy compared with those without the improvement of hypertension. Decrease in PACs after the adrenalectomy was associated with improved hypertension even among patients with subclinical hypercortisolism who did not have primary aldosteronism at baseline, whereas baseline PAC was not associated with that outcome. We found no evidence that aldosterone is associated with systolic blood pressure among patients with overt hypercortisolism. These findings indicate that elevated aldosterone may contribute to the presence of hypertension and its improvement rate after the adrenalectomy for patients with subclinical hypercortisolism.
To the best of our knowledge, this is one of the first studies to assess the potential role of aldosterone in hypertension among patients with overt and subclinical hypercortisolism, during both pre- and postoperative phases. Since aldosterone- and cortisol-producing adenoma was reported in 1979 [23, 24], several studies have assessed the cortisol production in aldosterone-producing adenoma clinically and histologically [8-10, 25] and showed the correlation between the degree of glucocorticoid excess levels and metabolic markers including BMI, waist circumference, blood pressure, insulin resistance, and high-density lipoprotein [12]. Prior research suggested that aldosterone-producing adenoma might produce cortisol as well as aldosterone even when serum cortisol levels after DST is less than 1.8 µg/dL (50 nmol/L) [11]. Although these studies have focused on cortisol synthesis among patients with aldosterone-producing adenoma, little is known about aldosterone synthesis among patients with cortisol-producing adenoma. Given that patients with hypercortisolism tend to have therapy-resistant hypertension and electrolyte disorders [8], our findings may generate the hypothesis that aldosterone contributes to the incidence and severity of hypertension in patients with possible autonomous cortisol secretion; this warrants further investigation.
There are several mechanisms by which cortisol excess leads to hypertension, such as regulating endothelial nitric oxide synthase expression modulated by 11β-hydroxysteroid dehydrogenases [26], activating the mineralocorticoid receptor [27] and upregulating vascular endothelin-1 [28]. Moreover, hypercortisolism impairs the production of endothelial vasodilators, including prostacyclin, prostaglandins, and kallikreins [29]. Despite these potential mechanisms, the direct effect of cortisol may not be sufficient to explain hypertension in patients with hypercortisolism, particularly subclinical hypercortisolism, and the presence of cortisol and aldosterone coproducing adenoma indicates another potential pathway to induce hypertension through aldosterone excess. Aldosterone is a steroid hormone not only promoting sodium reabsorption and volume expansion but also activating the mineralocorticoid receptor in the kidney and nonepithelial tissues (eg, adipose tissue, heart, endothelial cells, and vascular smooth muscle cells) [30]. It also induces oxidative stress, inflammation, fibrosis, vascular tone, and endothelial dysfunction [31]; therefore, aldosterone excess could induce hypertension even when it is slightly elevated [32]. A recent multiethnic study showed that aldosterone levels within the reference range were associated with subclinical atherosclerosis partially mediated through elevated blood pressure [33]. These mechanisms support our results indicating the potential contribution of aldosterone to hypertension among patients with subclinical hypercortisolism.
This study had several limitations. First, we did not have information on the duration of cortisol excess and therefore the estimated effect of cortisol on hypertension in our study might have been underestimated. The duration of exposure to mild hypercortisolism may be one of the important drivers of cardiovascular and metabolic disorders including irreversible vasculature remodeling in patients with subclinical hypercortisolism [2]. Second, we did not have the genetic information of adrenal tumors including aldosterone-producing adenoma. Given the heterogeneity of aldosterone responsiveness to ACTH [34] and postoperative hypertension resolution rate across genetic mutations (eg, KCNJ5, ATP1A1, ATP2B3, CACNA1D, CTNNB1) [35], such information might affect our findings. Third, because of the nature of an observational study, we cannot rule out the unmeasured confounding. Fourth, because aldosterone and cortisol levels were measured at a single point, we may have a risk of mismeasurement. Moreover, when evaluating aldosterone levels, we used dihydropyridine calcium channel blockers to control hypertension based on the clinical guideline of primary aldosteronism in Japan; this might lower serum aldosterone levels. Fifth, because the present study was conducted at a single center, selection bias is inevitable [13]. Given that primary aldosteronism—one of the major causes of secondary hypertension—has still been underdiagnosed, partially because of insufficient recognition of clinical guidelines [36], our findings may indicate the importance of considering aldosterone when evaluating patients with subclinical hypercortisolism accompanied by hypertension. However, we need to carefully interpret the observed “prevalence” in this study because individuals potentially having subclinical hypercortisolism were likely to come to our hospital, which specializes the adrenal disorders, and thus the numbers do not reflect the prevalence in general population. The small number of resected adrenal glands with the evaluation of CYP11B2 expression in this study cohort also limits the prevalence estimation of primary aldosteronism. Finally, as we only followed up 1 year after the adrenalectomy, we could not evaluate the long-term resolution rate of hypertension. To overcome these limitations and generalize our findings, future molecular studies and multicenter longitudinal studies with sufficient individual datasets and longer follow-up are required.
In conclusion, plasma aldosterone concentrations were associated with systolic blood pressure and improvement rate of hypertension after the adrenalectomy among patients with subclinical hypercortisolism—possible autonomous cortisol secretion without clinical signs of overt Cushing syndrome. Our findings underscore the importance of considering aldosterone when patients have an adrenal tumor with possible autonomous cortisol secretion complicated with hypertension. Future molecular and epidemiological studies are warranted to identify the potential role of aldosterone in hypertension among patients with subclinical hypercortisolism, clarify how often these patients also have primary aldosteronism, and examine the clinical effectiveness of the intervention targeting aldosterone for such patients.
Funding
K.I. was supported by the Japan Society for the Promotion of Science (JSPS; 21K20900 and 22K17392) and The Japan Endocrine Society. Study sponsors were not involved in study design, data interpretation, writing, or the decision to submit the article for publication. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Conflicts of Interest
All of authors confirm that there is no conflict of interest in relation to this work.
Data Availability
Restrictions apply to the availability of some data generated or analyzed during this study to preserve patient confidentiality or because they were used under license. The corresponding author will on request detail the restrictions and any conditions under which access to some data may be provided.
Abbreviations
-
ARR
aldosterone-to-renin ratio
-
BMI
-
DST
dexamethasone suppression test
-
F
-
HPA
hypothalamus-pituitary-adrenal
-
PAC
plasma aldosterone concentration
-
PRA
© The Author(s) 2022. Published by Oxford University Press on behalf of the Endocrine Society.
This is an Open Access article distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs licence (
https://creativecommons.org/licenses/by-nc-nd/4.0/), which permits non-commercial reproduction and distribution of the work, in any medium, provided the original work is not altered or transformed in any way, and that the work is properly cited. For commercial re-use, please contact journals.permissions@oup.com
© The Author(s) 2022. Published by Oxford University Press on behalf of the Endocrine Society.
Filed under: adrenal, Cushing's | Tagged: adrenalectomy, aldosterone, hypertension, subclinical hypercortisolism | Leave a comment »







![Enrollment and follow-up of the study population after the adrenalectomy. aThe prevalence of patients with overt hypercortisolism and hypertension among this study population may be higher than in the general population and therefore needs to be carefully interpreted given that the study institute is one of the largest centers for adrenal diseases in Japan. bAll patients in this category showed autonomous cortisol secretion (ie, serum cortisol levels >5.0 µg/dL [138 nmol/L] after a 1-mg dexamethasone suppression test). cOne case underwent adrenalectomy at another hospital and therefore no information was available after the adrenalectomy. dThe adrenalectomy was performed for 33 patients who were expected to improve their clinical symptoms and/or metabolic disorders, including hypertension. This assessment was mainly based on autonomous cortisol secretion evaluated by a 1-mg dexamethasone suppression test, complicated metabolic disorders, and autonomous aldosterone secretion evaluated by adrenal venous sampling for patients who were positive for the screening and confirmatory tests of primary aldosteronism. Details in the assessment can be found in the Methods section or elsewhere [18-20].](https://oup.silverchair-cdn.com/oup/backfile/Content_public/Journal/jes/7/1/10.1210_jendso_bvac167/2/m_bvac167f1.jpeg?Expires=1673226229&Signature=lH6Fo2svnZ4zLJ1vgDEWEShEHMnJYbw7JNP1Va6L~hR1SEu38yoBriwSZN9YHqMv3KcleFNJHIJun5Q0YYsBF9KclE-FpKJ0hmyzTCE6ZPxtRFpYNYDFSPY~4HTccGaYS6NvslM7g4mleOc1ZalfFRPRAzNZAeIvsLeaKXeF4pXP5dqL0W1jT-SgLyVkPbVhteCGMSm4fLytXM85yaB0AhExA3WwQuihmQU1sYbI0BeOE5tneusxGAFbxZDx2CbCT1UuYvaYHNAYQ6Q7NHMF2cpE0fW9HSkUpejOb5zgycvPAFaPiWmDZxoHDDhCIVzuUFpr7ngYe7MoS2O-QKd6tA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)