Abstract
Cushing disease is caused by excess ACTH secretion by a pituitary adenoma leading to hypercortisolism. Cyclic Cushing syndrome, in which periods of cortisol excess are interspersed by periods of normal or low values, poses a challenge to diagnostic testing and postoperative monitoring. We present a 26-year-old woman with cyclic Cushing syndrome who achieved apparent biochemical remission after transsphenoidal resection of an ACTH-producing pituitary tumor, confirmed on pathology. Despite initial clinical improvement, she later experienced recurring symptoms. Biochemical evidence of hypercortisolism was documented, but 1 month later morning serum cortisol was undetectable. A desmopressin stimulation test (DesST) produced a rise in ACTH and cortisol, indicating likely residual tumor tissue. After repeat surgery, pathology again confirmed an ACTH-secreting tumor. Postoperatively, ACTH and cortisol levels were again low, but a repeat DesST was now negative, suggesting successful resection of the residual tumor, and she remains in remission 3 years later. This case describes the unique utility of the DesST to detect a pituitary corticotroph tumor in cyclic Cushing disease during periods of low disease activity. It also highlights the potential role of the DesST in postoperative monitoring.
Introduction
Cushing disease (CD), in which excess ACTH from a pituitary adenoma drives hypercortisolism, causes up to 70% of endogenous Cushing syndrome (CS) [1]. When possible, the first-line treatment for CD is transsphenoidal surgery (TSS) to remove the causative tumor. This leads to remission in approximately 80% of cases, with recurrence rates estimated at 20% [2].
Cyclic CS, in which periods of excess cortisol are interspersed with periods of normal or low cortisol, complicates both the initial diagnosis of CS and the interpretation of post-TSS hormone levels [3]. Basal ACTH and cortisol, and dexamethasone suppression tests performed during a period of low disease activity, can be misleading because they reflect healthy pituitary corticotrophs that are responsive to and suppressed by persistent hypercortisolism [4]. The same mechanism of corticotroph suppression pertains after TSS, so that very low morning plasma ACTH and serum cortisol levels (generally less than 10 pg/mL [SI: 2.2 pmol/L] and 5 µg/dL [SI: 138 nmol/L], respectively), indicate successful tumor resection [5, 6]. However, if postoperative testing occurs during a period of low disease activity in cyclic CS, it may falsely indicate remission.
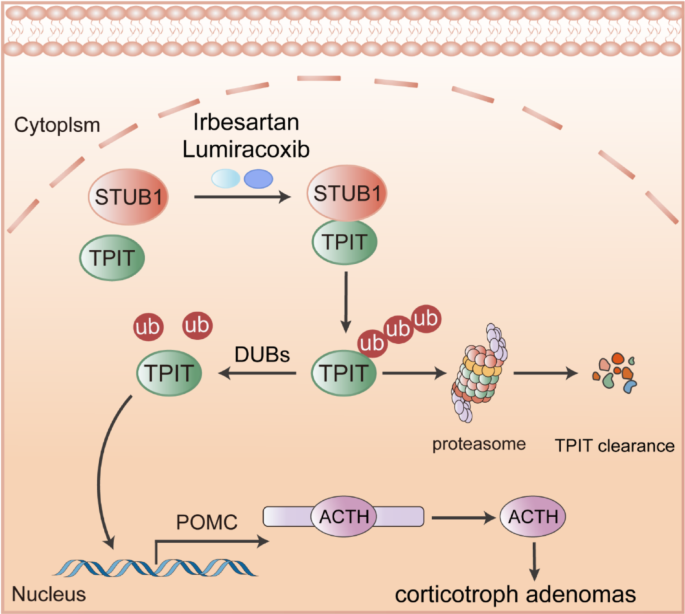
The desmopressin stimulation test (DesST), in which ACTH and cortisol levels are measured following intravenous administration of 10 µg desmopressin, may help to resolve these problems. Most corticotroph adenomas respond to desmopressin with an increase in ACTH secretion, followed by a cortisol increase [7, 8]. By contrast, most healthy people do not respond. Desmopressin, a synthetic analogue of arginine vasopressin (AVP), is believed to trigger this response by binding to upregulated V3 receptors or ectopically expressed V2 receptors on corticotroph adenomas [9]. Some of the most commonly used response criteria for the DesST, ≥35% and ≥20% increases in ACTH and cortisol, respectively, are based on thresholds that produce high performance for the CRH stimulation test [10]. Currently, however, there is no clear consensus on optimal cutoffs for the DesST [9].
The return of a positive DesST response has been shown to precede the return of hypercortisolism when monitoring for recurrence of CD [11]. By analogy, we postulated that a postoperative DesST might identify residual tumor in a patient with cyclic CS. In this case presentation, we will highlight the utility of the DesST to establish both partial and successful tumor resection in such a patient.
Case Presentation
A 26-year-old woman developed irregular menses, hair loss, facial rounding, a dorsocervical fat pad, and wide violaceous abdominal striae, accompanied by an unexplained 30-pound weight gain over 3 months. Over the same period, she also noted worsening of longstanding fatigue, anxiety, depression, and acne. Eventually, 1 year after these symptoms started, she was diagnosed with CS based on elevated midnight serum cortisol (24.5 µg/dL [SI: 675 nmol/L], reference range [RR]: <7.5 µg/dL [<207 nmol/L]), 24-hour urine free cortisol (UFC) (337 µg/day [SI: 931 nmol/day], RR: 3.5-45 µg/day [SI: 9.7-124 nmol/day]), and failure to suppress serum cortisol during a 48-hour low-dose dexamethasone suppression test (48-hour cortisol: 26.7 µg/dL [SI: 736 nmol/L], RR: <1.8 µg/dL [SI: <50 nmol/L]). ACTH was not suppressed and pituitary magnetic resonance imaging (MRI) revealed a right-sided 7 mm microadenoma. Bilateral inferior petrosal sinus sampling showed a high central-to-peripheral ACTH ratio, indicative of CD.
Because of surgical delays related to the COVID-19 pandemic, she was started on a block-and-replace regimen of metyrapone and hydrocortisone (HC) before undergoing TSS 6 months later, removing a tumor located in the right superior posterior portion of the pituitary. Pathology confirmed a pituitary tumor with diffuse positivity for ACTH, rare positivity for GH and prolactin, and low mitotic activity (Ki67 index <3%). Morning serum cortisol dropped to 1.2 µg/dL (SI: 33 nmol/L) (RR: 3.7-19.4 µg/dL [SI: 102-535 nmol/L]) on postoperative day 4, at which point physiologic HC replacement was started. HC was eventually tapered and stopped 8 months later, when morning serum cortisol had recovered. Postoperatively, her acne and menstrual irregularities resolved while hair loss continued and her weight stabilized without any significant reduction.
Later, she again developed worsening anxiety and a severely depressed mood to the point where she could barely function at her job. Because of these worsening symptoms, repeat testing was performed 10 months after surgery, confirming return of hypercortisolism: midnight serum cortisol 20.5 µg/dL (SI: 565 nmol/L), UFC 82 µg/day (SI: 227 nmol/day). A small lesion was seen on pituitary MRI, thought to represent postoperative changes or a residual adenoma.
Diagnostic Assessment
The patient presented to our institution for a second opinion. A pituitary MRI was unchanged from the month prior. Unexpectedly, laboratory values now showed undetectable bedtime salivary (<50 ng/dL [SI: 1.4 nmol/L], RR: <100 ng/dL [SI: <2.8 nmol/L]) and morning serum cortisol (<1 µg/dL [SI: <27.6 nmol/L]), and low-normal ACTH (11.9 pg/mL [SI: 2.6 pmol/L], RR: 5.0-46.0 pg/mL [SI: 1.1-10.1 pmol/L]), and UFC (5.6 µg/day [SI: 15.5 nmol/day]). She did not have clinical symptoms of adrenal insufficiency. These results, indicative of secondary adrenal insufficiency, were in stark contrast to the hypercortisolism confirmed 1 month earlier, raising suspicion for apoplexy of residual tumor tissue or cyclic CS. Upon further questioning, the patient reported previous waxing and waning of acne severity, but no clear cyclicity of other symptoms. She felt that it was not possible for her to assess emotional or cognitive variability apart from that caused by the COVID-19 pandemic. Three weeks later, she underwent a DesST, during which baseline cortisol and ACTH were 3.1 µg/dL (SI: 86 nmol/L) and 34.1 pg/mL (SI: 7.5 pmol/L), respectively. After desmopressin, ACTH increased +111% at +15/30 minutes and cortisol increased +172% at +30/45 minutes (Fig. 1). This positive response was interpreted as confirming the presence of residual tumor tissue.

ACTH and cortisol responses during the desmopressin stimulation test (DesST) before and after the patient’s second transsphenoidal surgery. Plasma ACTH (A) and serum cortisol (B) levels were measured twice at baseline before and 15, 30, 45, and 60 minutes after intravenous administration of 10 µg desmopressin. Circles and squares represent the values from tests performed before and after surgery, respectively. The presence of a response (despite a low baseline cortisol level) in the preoperative test was considered to represent residual corticotroph tumor tissue; the postoperative loss of response to desmopressin was thought to represent successful resection of residual tumor.
Treatment
Two weeks after the positive DesST, on admission for repeat TSS, morning serum cortisol had risen to 15.2 µg/dL (SI: 419 nmol/L). After resection of residual tissue within the anteroinferior and right lateral aspect of the gland, pathology again confirmed a focus of ACTH-positive tumor. By postoperative day 3, morning serum cortisol was again undetectable with an unchanged plasma ACTH of 12.1 pg/mL (SI: 2.7 pmol/L). Because of the difficulty in distinguishing a satisfactory postoperative biochemical response from a period of low disease activity in cyclic CS, a second DesST was performed. This time the test was negative, with ACTH increasing by only 8%, whereas cortisol remained undetectable throughout (Fig. 1). This drastic change in response to desmopressin was believed to represent successful resection of residual tumor tissue. She was discharged on physiologic HC replacement and daily desmopressin after developing postoperative AVP deficiency.
Outcome and Follow-up
The AVP deficiency resolved over 6 months, whereas HC was stopped after 8 months, following a normal insulin tolerance test. The patient lost 20 pounds in the first 9 months after her second surgery, before gradually losing an additional 40 pounds over the following 3 years, reaching her baseline weight. The facial rounding and dorsocervical fat pad resolved, and acne improved. Three years after her second surgery, biochemical remission was maintained but she continued to experience hair loss, reduced taste and smell, and fluctuating severity of her preexisting fatigue, anxiety, and depression.
Discussion
Of note, our patient’s initial evaluation and surgery took place at an expert pituitary center in the United Kingdom, whereas the second evaluation was performed in the United States. This case shows some regional differences in testing protocols; for example, the 48-hour dexamethasone suppression and insulin tolerance tests are used more often in the United Kingdom. However, both surgical procedures were performed by high-volume pituitary surgeons, which is crucial to maximize the probability of remission [2].
While previous reports have described the role of the DesST in CD diagnosis [9], our case highlights its unique utility during periods of low disease activity in cyclic CD. Other tests for the diagnosis or etiology of CS rely on ongoing disease activity and require ongoing tumoral secretion of ACTH accompanied by suppression of healthy corticotrophs. Importantly, most healthy corticotrophs do not exhibit a significant response to desmopressin [7, 9]. In our patient, the diagnosis of CD was confirmed based on previous surgical pathology. Although documented recurrent hypercortisolism and CS symptoms were highly suspicious, the presence of residual disease was questioned due to the lack of ongoing hypercortisolism. In this context, the clearly positive response to DesST provided supportive evidence for pursuing a second TSS. The subsequent postoperative loss of response to desmopressin was interpreted as representing successful resection of all residual tumor tissue, which was supported by enduring remission of most symptoms 3 years after surgery. Biochemical postoperative assessments are based on trends in ACTH and cortisol. Typically, both hormones plummet after successful removal of an ACTH-producing tumor, since healthy corticotrophs remain suppressed because of longstanding hypercortisolism. Corticotrophs take at least 6 months to recover; earlier normalization of ACTH and cortisol raises concern for residual tumor tissue [12].
Postoperative hormonal trends may be different in 2 settings that were both relevant to our patient: preoperative medical therapy to restore eucortisolism and cyclic CS. In both scenarios, recent hypercortisolism may have been mild or absent, potentially allowing for a swift recovery of healthy corticotrophs. Postoperative ACTH and cortisol levels may be normal, making it difficult to establish a biochemical cure. In this setting, the usual screening tests for hypercortisolism (UFC, bedtime cortisol, low-dose dexamethasone suppression test) are useful to determine whether excessive ACTH secretion persists.
However, these postoperative screening tests for hypercortisolism may not be reliable in cyclic CS since low or normal ACTH and cortisol levels can reflect either remission or low disease activity. The DesST may be particularly useful in this situation to identify residual disease or confirm successful tumor resection. For this test to be useful, however, it is important to obtain a preoperative DesST to establish a baseline because a minority of tumors causing CD do not respond to desmopressin [9].
Learning Points
-
Most healthy pituitary corticotrophs and tumors causing ectopic ACTH syndrome do not exhibit a response during the desmopressin stimulation test (DesST), making it useful for Cushing disease (CD) diagnosis.
-
The DesST may be particularly useful during periods of low disease activity in cyclic Cushing syndrome, as other dynamic tests used to diagnose CD may be uninterpretable in this setting.
-
Postoperatively, the DesST may be useful to confirm successful tumor resection and to monitor for CD recurrence. It is, however, important to obtain a preoperative DesST to establish whether the causative tumor is responsive to desmopressin.
Contributors
All authors made individual contributions to authorship. B.M.B., L.K.N., and H.E. were involved in the writing and submission of the manuscript. W.D., R.M., L.K.N., and H.E. were involved in the diagnosis and management of this patient. All authors reviewed and approved the final draft.
Funding
This research was supported by the Intramural Research Program of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) within the National Institutes of Health (NIH). The contributions of the NIH authors were made as part of their official duties as NIH federal employees, are in compliance with agency policy requirements, and are considered Works of the United States Government. However, the findings and conclusions presented in this paper are those of the authors and do not necessarily reflect the views of the NIH or the U.S. Department of Health and Human Services.
Disclosures
B.M.B., W.D., R.M., and H.E. have nothing to disclose. L.K.N. receives royalties from UpToDate.
Informed Patient Consent for Publication
Signed informed consent obtained directly from the patient.
Filed under: Cushing's, pituitary, Rare Diseases | Tagged: ACTH, Cyclical Cushing's, desmopressin stimulation test, hypercortisolism, pituitary | Leave a comment »