Jokichi Takamine was a Japanese-American biochemist and industrialist, born Nov. 3, 1854, who isolated the hormone produced in the adrenal gland that causes the body to respond to emergencies. This chemical was adrenalin — now called epinephrine — from the suprarenal gland. It was the first pure hormone to be isolated from natural sources.
He applied for and received a U.S. patent on the substance, and went on to make a fortune with his marketing of Adrenalin. In fact, the product that he marketed was not pure epinephrine, but a mixture of the hormone and its sibling compound, norepinephrine, or noradrenaline. It is now made synthetically. He also found takadastase, and played a key role in the introduction of phosphate fertilizer along with various other manufacturing and chemical industries to Japan.
~~~~~
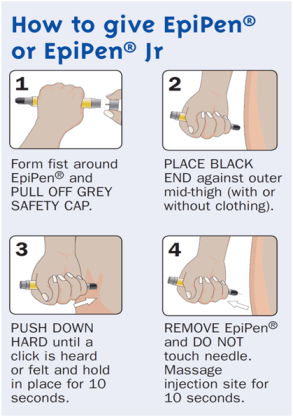
Epinephrine, an EpiPen or Auvi-Q/Allerject injection, should be given in the mid-anterior lateral thigh (not the outer thigh). We call this the EpiCenter of the thigh, and this video segment from the EpiCenter Medical (http://www.epicentermedical.com) online anaphylaxis first aid course has a thigh location graphic to help you pinpoint the most effective location for the injection.
Filed under: adrenal, adrenal crisis, Video | Tagged: adrenal crisis, Adrenal gland, adrenalin, anaphylaxis, epinephrine, EpiPen, Hormone, injection, noradrenaline, suprarenal gland, video | Leave a comment »