PET/MRI could become the diagnostic method of choice over MRI alone for identifying small pituitary tumors associated with Cushing disease, according to a study published March 21 in the Journal of Nuclear Medicine.
In patients diagnosed with the disease yet who had inconclusive MRI results, PET/MRI was positive in 100% of cases, noted lead author Ilanah Pruis, a doctoral student at Erasmus University Medical Center in Rotterdam, Netherlands.
“This multimodal imaging technique provides a welcome improvement for diagnosis, planning of surgery, and clinical outcome in patients with Cushing disease,” the authors wrote.
Cushing disease is characterized by small tumors in pituitary glands, which causes them to secrete excess cortisol, the authors explained. While it is a rare disease, over time it can cause severely disabling conditions, such as high blood pressure or type II diabetes.
Currently, guidelines recommend the use of MRI and inferior petrosal sinus sampling (IPSS) to diagnose these tumors. IPSS is an invasive procedure in which cortisol hormone levels are sampled from the veins that drain the pituitary gland.
In up to 40% of patients, however, MRI is inconclusive, as the lesions are smaller than 10 millimeters in diameter. Even advanced MRI techniques, such as dynamic perfusion imaging, can leave small lesions undetected in up to one third of patients, the authors noted.
In preclinical work, PET imaging using a radiotracer named F-18 FET has been shown to bind with high affinity to a molecular target in pituitary tumors, and in this study, the researchers aimed to test this technique combined with MRI in a multimodal approach.
The researchers analyzed results from 22 patients (68% women; mean age 48 years) who underwent F-18 FET PET/MRI at Erasmus MC between February 2021 and December 2022. All patients showed a clear pituitary tumor F-18 FET-PET/MRI, whereas reading of the MRI alone yielded a suspected lesion in only 50%, the authors found.
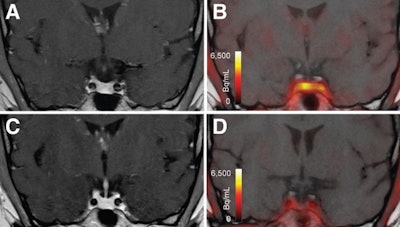 T1-weighted postgadolinium MR images (A and C) and F-18 FET-PET/MR images (B and D) centered at pituitary before (A and B) and after (C and D) transsphenoidal surgery. This patient with Cushing disease showed clear focal uptake (B) but no clear lesion on previously obtained and accompanying MRI (A). Postoperative tissue analysis did confirm resection of small pituitary adenoma/PitNET, and postoperative F-18 FET-PET showed no residual uptake (D). Image courtesy of the Journal of Nuclear Medicine.
T1-weighted postgadolinium MR images (A and C) and F-18 FET-PET/MR images (B and D) centered at pituitary before (A and B) and after (C and D) transsphenoidal surgery. This patient with Cushing disease showed clear focal uptake (B) but no clear lesion on previously obtained and accompanying MRI (A). Postoperative tissue analysis did confirm resection of small pituitary adenoma/PitNET, and postoperative F-18 FET-PET showed no residual uptake (D). Image courtesy of the Journal of Nuclear Medicine.
Importantly, 16 patients underwent treatment based on the results — either surgery, Gamma Knife, or CyberKnife therapy — with 12 of these patients achieving short-term remission, the authors noted.
“[F-18 FET-PET/MRI] is of great clinical value because it allows precision surgery and targeted Gamma Knife or CyberKnife therapy,” the group wrote.
The researchers noted that only one previous study evaluated F-18 FET-PET/MRI in these patients and that their study was limited, given the relatively small number of patients.
“Future studies will be directed at head-to-head comparisons of the performance of F-18 FET- PET and other diagnostic techniques, including advanced MRI sequences… preferably in patients at the time of initial clinical presentation,” the authors concluded.
A link to the full study can be found here.
From https://www.auntminnie.com/clinical-news/molecular-imaging/article/15667496/petmri-may-improve-diagnosis-of-cushing-disease
Filed under: Cushing's, Diagnostic Testing, pituitary | Tagged: F-18 FET, Inferior petrosal sinus sampling, IPSS, Journal of Nuclear Medicine, PET/MRI, pituitary tumors | Leave a comment »






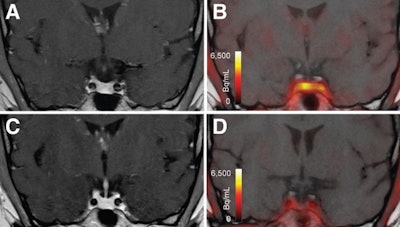 T1-weighted postgadolinium MR images (A and C) and F-18 FET-PET/MR images (B and D) centered at pituitary before (A and B) and after (C and D) transsphenoidal surgery. This patient with Cushing disease showed clear focal uptake (B) but no clear lesion on previously obtained and accompanying MRI (A). Postoperative tissue analysis did confirm resection of small pituitary adenoma/PitNET, and postoperative F-18 FET-PET showed no residual uptake (D). Image courtesy of the Journal of Nuclear Medicine.
T1-weighted postgadolinium MR images (A and C) and F-18 FET-PET/MR images (B and D) centered at pituitary before (A and B) and after (C and D) transsphenoidal surgery. This patient with Cushing disease showed clear focal uptake (B) but no clear lesion on previously obtained and accompanying MRI (A). Postoperative tissue analysis did confirm resection of small pituitary adenoma/PitNET, and postoperative F-18 FET-PET showed no residual uptake (D). Image courtesy of the Journal of Nuclear Medicine.





