Fabiana had transsphenoidal surgery (pituitary) July 30th 2004. She had a recurrence after seven years of being Cushing’s free. A second pituitary surgery on 10/26/2011 was unsuccessful.
Another Golden Oldie, this bio was last updated 9/12/2015

Fabiana will be our guest in an interview on BlogTalk Radio Wednesday, October 21 at 6:00 PM eastern. The Call-In number for questions or comments is (657) 383-0416.
The archived interview will be available after 7:00 PM Eastern through iTunes Podcasts (Cushie Chats) or BlogTalkRadio. While you’re waiting, there are currently 88 other past interviews to listen to!
~~~
Well it has taken me a year to write this bio…and just to give some hope to those of you just going thru this process…I have to say that after surgery I have not felt better! I am back to who i always knew I was….the depression and anxiety is gone and I am living life like a 24 year old should!
I guess it all started when i was sixteen (hindsight is 20-20 i guess). My periods stopped i was tired all the time and the depression started. We all kind of just chalked it up to being sixteen. But my mom insisted something was not right. we talked with my gyno…who said nothing was wrong, I had a fungus on my head (my hair was getting really thin) and sometimes girls who had normal periods (in my case three years of normal periods) just go awry.
My mom wasnt hearing that and demanded a script for an endo. I went….he did blood work…and metioned cushings. But nothing came back definitive…so they put me on birthcontol and gave me some hormones and the chushings was never mentioned again because that all seemed to work.
As time went on my depression got worse, the shape of my body started to change-my face and stomach was the most noticeable- and my energy level kept going down. I kept going back to the doctors asking to be tested for mono..or something. I went to a psycologist….but i knew there was no reason for my depression. Two of them told me “i had very good insight” and that I didnt need them. I started getting more anxiety..especially about going out socially.
High school ended and my typical optimistic personality started to decline. I put on a good act to my friends but my family was seeing me break down all the time. I went away for college (all the while gaining weight). My sophmore year I had a break down..I called my family crying that i needed help. I couldnt beat my depression. I didnt drink in college because i knew that would mean instant weight gain, i barely went out…i exercised everyday..hard….i joined weight watchers…i stuck with it. I was at 103 lbs….that crept up to 110…that crept up to 117…each time my weight goal would be “ohh if i could just get back to 108..112…115” with each weight gain my original weight goal would get higher and higher.
Internally i felt like I was constantly under a black cloud..i knew there was no reason why i shoudl feel this way..i was doing great in school, i had a supportive family, an amazing boyfriend and great friends…why was i depressed? I was becoming emotionally draining to the people closest to me…I would go home a lot on the weekends…i was diagnosed with PMDS….like severe PMS..and was given an antidepresant…i hated it it made me feel like a zombie…i stopped taking it and just made it apoint to work on fighting the depression….and the weight gain.
When i was done college i was about 120 lbs. My face was getting rounder and rounder..i was noticing more hair on my face and arms…and a hump between my shoulder blades and the bottom of my neck. My mom saw a tv show about Polycystic ovarian syndrome and felt that maybe that was what was going on with me…i went to my PCP with this and she said it was possible and that i should to talk to my gyno….I am 4’8 and at the time weighing close to 125..i talked to my gyno and she said I was not heavy..that i was just “itailan” ..i told her my periods were getting abnormal again even w/the birthcontrol and that i was so tired all the time and my arms and legs ached. I also told her that i was bruising very easily…and that the weight gain would not stop despite my exercising and following the atikins diet very strickly for over 6 weeks. My boyfriend and I decided to try the diet together..he lost 35 llbs in 6 weeks..i lost NOTHING! I went back to my PCP who ordered an ultra sound of my ovaries…..NOTHING.(i kept thinking i was going crazy and that it was all in my head)….she also decided to do some blood work…and as i was walking out the door she said..”you know what..i am going to give you this 24hr urine test too. Just so that we cover everything”. I just kept thinking please let something come back ….please dont let this be all my fault…please dont let this be all in my head…..please dont let me be crazy. When i got the test results back it turned out that the 24hr urine test was the one test i needed to get on the right track to finding what was wrong. My cortisol level was 3x’s the normal.
I went to an endo…by the time i got to the endocronoligist i was up to 130…i could not work a full day without needing a full day of sleep and my body was aching beyond description. I was crying all the time…in my room…and was becoming more and more of a recluse…i would only hang out with my boyfriend in our houses. I looked my symptoms up on the internet and saw cushings…that was it! I went to the endo and told him..i think it is cushings….he said he had only saw it one other time and that he wanted to do more tests. I got CAT scans, x-rays, MRI’s….my adrenals my pituitary my lungs….he did a CRH stimulation test which was getting blood work done every fifteen minutes for 90minutes….it took weeks to get that test scheduled..no one had ever heard of it and therefore did not know how to do it…..finally after 3 months of tests my dr. felt he had enough evidence to diagnos me with cushings disease (tumor on my pituitary) I was diagnosed in March of 2004. By this time i was about 137 lbs i had to work part time (i am an occupational therapist for children..i do home visits….i could not make it thru a whole day)
In April i had to change to office work…i could not lift the children and i could barely get up off the floor. I have to say i was one of the lucky people who worked for people who were very supportive and accomidating…my boss was very willing to work with me and willing to hold my job for me.
July 30th 2004 i finally had transphenodial surgery to remove my tumor (they went thru my lip and nose because they felt my nose was too small). It is now over 1 year later….i am down to 108 lbs, i have so much energy…no depression….and i dont mind looking at myself in the mirror…i am enjoying my friends and my boyfriend…(who stayed with me thru it all) And my family. I feel healthy mentally, emptionally, and physically. And i just got back into my size 2 jeans!!!
It was a crappy time…(as i am sure you all can atest to) but i learned a lot…..most importantly i was bombarded by good wishes and prayers….friends requested masses for me…a nun in brazil prayed for me…people who i never thought i touched their lives…took the time to wish me well…send an email..or call….I got to experience the wonderful loving nature of human beings and i was lucky to be supported by my family (my mom, dad, and two younger brothers) and my boyfriend throughout this entire tough journey.
This experience taught me to realize the strength i have as well as to appreciate the good and the bad in life. I was on hydrocortizone for about 8 months…i was lucky that my tumor was in its own little sack so my pituitary gland was not touched. In the end in took about 7 years to diagnose me..i think that if the dr. at 16 would have pursued the cushings idea nothing would have been found because it took so long for my symptoms to really peak…needless to say i love my PCP and my endo ..and that i changed gyno’s…
I just want to let anyone out there going thru this disease to know..you are not alone….and to take each day is stride…when you need help ask for it….and that this road can lead to a happy ending. God Bless!
ps- it is ok to feel bad about what you are going thru…it is a tough thing to endure…and when the docotors tell you there is noting wrong…..follow your gut…and you keep searching for the doctor that will listen… If there is anyone in the philadelphis of south jersey area who needs someone to talk to please feel free to email me…fapadula@hotmail.com…i will help you out the best i can!
Update November 6, 2011
Well- here is an update, after seven years of being Cushings free it has returned.
With in those seven years I married my college boyfriend and we now have a son- Nicholas who will be 2 in Decemeber. It has been a blessed and wonderful seven years. However right around when my son was turning 1 I started to notice symptoms again. Increase facial hair, the whole “roundness” of my body, buffalo hump. I decided I was going to work out hard, eat right, and see – I didnt just want to jump to any conclusions. I stuck to it- and nothing…..my hair started thinning again and the acne was coming back and then the missed periods…..so I went to my PCP- told them i needed the 24hr urine and wouldnt you know…..427 cortisol level (on that 0-50 scale)……here we go again.
So back to endo- now at Penn Pituitary Center…..it was another journey b/c the tumor wasnt definative on MRI, and it seems to be cycling…..but I was diagnosed with Cushings again- with the option of 2nd pit surgery or BLA…….after some months of trying to make a decision I went with the 50/50 chance of the second pituitary surgery on 10/26/2011.
It didnt work- my levels never came down in the hospital and I went home w/ out of range cortisol levels and no need for medication……BLURG……Sooooo on to the next step…..after I recover from this surgery I will most likely have the BLA- with the hopes of not having to deal with Cushings ever again. This time around has been a little more difficult just with being a mom and feeling sick- but I still continue to be amazingly blessed with a supportive family and husband and we are surrounded by love and support and for that I am beyond greatful.
I keep all of you in my prayers for relief and health- as I ( we all) know this no easy journey.
Many Blessings!
Fabiana
Update September 12, 2015
So to bring this up to date. My second pituitary surgery in 2011 was unsuccessful. January of 2012 I had both of my adrenal glands removed. Going to adrenal insufficiency was a very difficult transition for me. It took me nearly 2 years before I felt functional. As time went on I felt more human, but I haven’t felt healthy since that day. I can and do function, but at a lower expectation of what I used to be capable of….my “new normal”.
My husband and I decided to try for a second child…my pituitary was damaged from the second surgery and we needed fertility…after 8 months of fertility I got pregnant and we had our second son January of 2015.
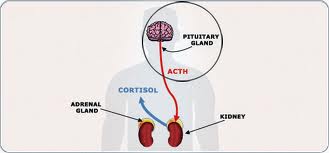
In April of 2015 we discovered that my ACTH was increasing exponentially. MRI revealed a macroadenoma invading my cavernous sinus. The tumor is sitting on my carotid artery and milimeterrs away from my optic chasim. I was not a candidate for another surgery due to the tumors proximity to.both of those vital structures.
So September 1st of this year I started daily radiation treatments. I spent my 34th birthday getting my brain zapped. I am receiving proton beam therapy at the Hospital of the University of Pennsylvania. I am so lucky to live so close to an institute that has some of the rarest treatment options.
Again Cushing’s is disrupting our life, my husband goes with me every night to radiation while family takes turns watching the kids….I am now on my 18th year of fighting this disease. I never imagined it would get to this point.
But here we all are making the best of each day, fighting each day and trying to keep things as “normal” as possible. Blessings to all of you fighting this disease…my new go to saying is” ‘effing Cushing’s”! For you newbies…Fight, Advocate for yourselves, and find a doc who doesn’t dismiss you and hang on to them for dear life.
HOME | Sitemap | Adrenal Crisis! | Abbreviations | Glossary | Forums | Donate | Bios | Add Your Bio | Add Your Doctor | CushieWiki
Filed under: Cushing's, Interview, pituitary, Rare Diseases, Treatments | Tagged: 24-hour urinary free cortisol, adrenal, anxiety, BLA, bloodwork, bruising, buffalo hump, cortisol, CRH stimulation, CT scan, Cushing, Cushing Syndrome, depression, diagnosis, energy, fungus, Golden Oldie, hair loss, hirsuitism, hydrocortisone, lungs, Magnetic resonance imaging, March 2004, moonface, MRI, periods, pituitary, Pituitary gland, PMDS, PMS, Polycystic ovary syndrome, recurrence, sleep, transsphenoidal, UFC, ultrasound, Weight gain, X-ray computed tomography, X-rays | Leave a comment »