Pituitary tumors can vary widely in severity, with some requiring surgical intervention. While certain pituitary tumors are more straightforward to remove, those that extend beyond the medial wall of the cavernous sinus (MWCS) are considered complex. A delicate region near the pituitary gland, the MWCS contains critical structures like cranial nerves and the carotid artery, which present additional surgical challenges.
Historically, surgeons avoided entering the cavernous sinus due to the risk of damaging these vital structures, but new advancements have made it possible to remove tumors more effectively and safely. Innovative surgical techniques, such as endoscopic endonasal approaches, are allowing neurosurgeons to navigate these delicate areas with greater precision and confidence than ever before.
Neurosurgeon Dr. Kaisorn Chaichana, who has performed well over 100 such procedures at Mayo Clinic in Jacksonville, Florida, says, “The latest advancements in pituitary surgery are driven by improved camera optics. Angled scopes now let us see around corners, helping us distinguish the pituitary gland from the tumor with far greater precision than traditional microscopes. Doppler and ultrasound also allow us to identify critical structures like the carotid artery, ensuring safer, more complete tumor removal.”
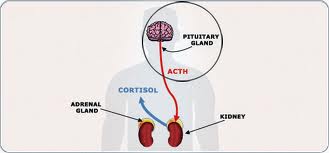
If a tumor that extends into the MWCS is not removed, it may continue producing excessive hormones, leaving patients with persistent symptoms. “It’s almost as if they didn’t have surgery at all because there’s still that tumor there causing that hormonal imbalance. That’s why achieving total removal is so critical for long-term success,” said Dr. Chaichana.
Although the procedure is not entirely new, widespread adoption is relatively recent, and only a few institutions perform this surgery regularly. The complexity of the procedure requires expert knowledge of the surrounding anatomy, as well as careful coordination between neurosurgeons, ear, nose, and throat (ENT) specialists, and post-operative care led by an endocrinologist. “The cavernous sinus is an area a lot of surgeons aren’t comfortable with, and that’s why we specialize in that surgery here,” added Dr. Chaichana. Mayo Clinic’s multidisciplinary approach has improved patient outcomes, allowing for safer tumor removal with reduced complications.
For patients with recurrent tumors or those initially deemed inoperable, re-evaluating surgical options at a specialized center may provide new hope. If the tumor is confined to one side of the carotid artery, surgeons can often achieve a complete resection. However, if it extends beyond this point, additional treatments such as radiation or medical therapy may be required.
Patients facing pituitary surgery should seek a neurosurgeon with experience in endoscopic techniques at a specialized facility with extensive expertise in pituitary tumor treatment.
Choosing the right surgical team can significantly impact outcomes, particularly for complex cases. While not all tumors require MWCS resection, for those that do, this approach offers a path to better surgical success and long-term remission. With ongoing advancements in pituitary surgery, more patients than ever have access to safer, more effective treatment options.
For more information or to request an appointment, please visit Pituitary Tumor Care – Mayo Clinic
Filed under: Cushing's, pituitary, Treatments | Tagged: cavernous sinus cavity, Dr. Kaisorn Chaichana, endocrinologist, Mayo Clinic, neurosurgeon, pituitary, tumor | Leave a comment »