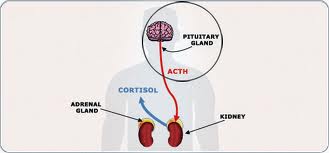
A condition in which the body produces too much cortisol, Cushing’s disease occurs when a tumor on the pituitary gland makes the gland create too much ACTH, the hormone that stimulates the production and release of cortisol (also known as “the stress hormone”). It may also occur with excess growth of the pituitary gland, known as hyperplasia. For most patients, Cushing’s disease will show itself through symptoms like red lines on the abdomen, abdominal weight gain and roundness to the face. And while the condition only affects 10 to 15 people per million per year, patients who suffer with it understandably wonder why. What are the causes? Where would a pituitary gland tumor come from? What leads to excess growth of that gland? To help answer these questions, here’s a look at Cushing’s disease causes:
Causes of Cushing’s Disease
The most common cause for Cushing’s disease is adenoma, a usually benign tumor on the pituitary gland. Because the tumors are normally pretty small, they can be hard to diagnose. For this reason, many patients who have Cushing’s disease don’t find out right away. Meeting with an endocrinologist can help the diagnosis process, improving your chances for a fast, successful recognition of the disease.
Risk Factors for Cushing’s Disease
Even though it’s a rare condition, Cushing’s disease occurs more commonly in women, particularly those between the ages of 20 and 50. Other factors that may increase the risk of Cushing’s disease include obesity, type 2 diabetes, poorly controlled blood sugar levels and high blood pressure. While none of these factors are a direct cause of the condition, they are associated with higher prevalence of it.
Cushing’s Disease vs. Cushing’s Syndrome
Often mistaken for one another, Cushing’s disease and Cushing’s syndrome are actually not the same condition. What they have in common is that they both involve the body’s producing too much cortisol. Cushing’s disease is a medical condition, however, while Cushing’s syndrome is a symptom of it. Cushing’s syndrome will often occur when a patient is taking corticosteroid medication.
Why You Should See an Endocrinologist
If you believe you or someone you love may have Cushing’s disease, it is best to see a specialist. Symptoms develop slowly and sometimes in cycles, so without proper testing it can be hard to identify what’s happening. A skilled endocrinologist can conduct hormone blood tests to measure blood cortisol levels at different times. He or she can also schedule an MRI for an individual who is not taking cortisol medications, in order to isolate the location of any tumors.
Have you been dealing with the symptoms of elevated cortisol levels, such as unexplained weight gain, particularly in the abdominal area and/or back of the neck? Is your skin or vision changing? These symptoms could be indicating a deeper problem in your body — so schedule an appointment to have your condition evaluated by a professional as soon as you can. Through proper treatment, you may be able to reduce or even eliminate your symptoms and be restored to full health again.
Filed under: Cushing's, FAQ, pituitary | Tagged: ACTH, cortisol, Cushing's Disease, MRI, pituitary, tumor, weight | 1 Comment »