In a recent study published in Hypertension Research, scientists examine the endocrine causes of hypertension (HTN) and investigate the efficacy of treatments to alleviate HTN.
What is HTN?
About 30% of the global population is affected by HTN. HTN is a modifiable cardiovascular (CV) risk factor that is associated with a significant number of deaths worldwide.
There are two types of HTN known as primary and secondary HTN. As compared to primary HTN, secondary HTN causes greater morbidity and mortality.
The most common endocrine causes of HTN include primary aldosteronism (PA), paragangliomas and pheochromocytomas (PGL), Cushing’s syndrome (CS), and acromegaly. Other causes include congenital adrenal hyperplasia, mineralocorticoid excess, cortisol resistance, Liddle syndrome, Gordon syndrome, and thyroid and parathyroid dysfunction.
What is PA?
PA is the most common endocrine cause of hypertension, which is associated with excessive aldosterone secretion by the adrenal gland and low renin secretion. It is difficult to estimate the true prevalence of PA due to the complexity of its diagnosis.
Typically, the plasma aldosterone-to-renin ratio (ARR) is measured to diagnose PA. The diagnosis of PA can also be confirmed using other diagnostic tools like chemiluminescent enzyme immunoassays (CLEIAs) and radio immune assay (RIA).
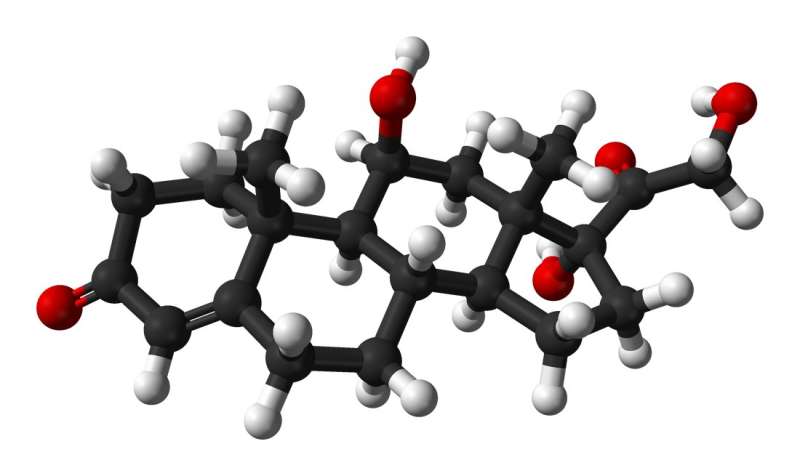
Continuous aldosterone secretion is associated with organ damage due to chronic activation of the mineralocorticoid (MR) receptor in many organs, including fibroblasts and cardiomyocytes. An elevated level of aldosterone causes diastolic dysfunction, endothelial dysfunction, left ventricular hypertrophy, and arterial stiffness.
Increased aldosterone secretion also leads to obstructive sleep apnea and increases the risk of osteoporosis. This is why individuals with PA are at a higher risk of cardiovascular events (CVDs), including heart failure, myocardial infarction, coronary artery disease, and atrial fibrillation.
PA is treated by focusing on normalizing potassium and optimizing HTN and aldosterone secretion. Unilateral adrenalectomy is a surgical procedure proposed to treat PA.
Young patients who are willing to stop medication are recommended surgical treatment. The most common pharmaceutical treatment for PA includes mineralocorticoid receptor antagonists such as spironolactone and eplerenone.
Pheochromocytomas and paragangliomas
PGL are tumors that develop at the thoracic-abdominal-pelvic sympathetic ganglia, which are present along the spine, as well as in the parasympathetic ganglia located at the base of the skull. The incidence rate of PGL is about 0.6 for every 100,000 individuals each year. PGL tumors synthesize excessive catecholamines (CTN), which induce HTN.
Some of the common symptoms linked to HTN associated with PGL are palpitations, sweating, and headache. PGL can be diagnosed by determining metanephrines (MN) levels, which are degraded products of CTN. Bio-imaging tools also play an important role in confirming the diagnosis of PGL.
Excessive secretion of CTN increases the risk of CVDs, including Takotsubo adrenergic heart disease, ventricular or supraventricular rhythm disorders, hypertrophic obstructive or ischaemic cardiomyopathy, myocarditis, and hemorrhagic stroke. Excessive CTN secretion also causes left ventricular systolic and diastolic dysfunction.
Typically, PGL treatment is associated with surgical procedures. Two weeks before the surgery, patients are treated with alpha-blockers. For these patients, beta-blockers are not used as the first line of treatment without prior use of alpha-adrenergic receptors.
Patients with high CTN secretion are treated with metyrosine, as this can inhibit tyrosine hydroxylase. Hydroxylase converts tyrosine into dihydroxyphenylalanine, which is related to CTN synthesis.
What is CS?
CS, which arises due to persistent exposure to glucocorticoids, is a rare disease with an incidence rate of one in five million individuals each year. The most common symptoms of CS include weight gain, purple stretch marks, muscle weakness, acne, and hirsutism. A high cortisol level causes cardiovascular complications such as HTN, hypercholesterolemia, and diabetes.
CS is diagnosed based on the presence of two or more biomarkers that can be identified through pathological tests, such as salivary nocturnal cortisol, 24-hour urinary-free cortisol, and dexamethasone suppression tests.
CS is treated through surgical procedures based on the detected lesions. Patients with severe CS are treated with steroidogenic inhibitors, such as metyrapone, ketoconazole, osilodrostat, and mitotane. Pituitary radiotherapy and bilateral adrenalectomy are performed when other treatments are not effective.
Acromegaly
Acromegaly arises due to chronic exposure to growth hormone (GH), leading to excessive insulin-like growth factor 1 (IGF1) synthesis. This condition has a relatively higher incidence rate of 3.8 million person-years. Clinical symptoms of acromegaly include thickened lips, widened nose, a rectangular face, prominent cheekbones, soft tissue overgrowth, or skeletal deformities.
Prolonged exposure to GH leads to increased water and sodium retention, insulin resistance, reduced glucose uptake, and increased systemic vascular resistance. These conditions increase the risk of HTN and diabetes in patients with acromegaly. Acromegalic patients are also at a higher risk of cancer, particularly those affecting the thyroid and colon.
Acromegaly is diagnosed using the IGF1 assay, which determines IGF1 levels in serum. After confirming the presence of high IGF1 levels, a GH suppression test must be performed to confirm the diagnosis. Bioimaging is also conducted to locate adenoma.
Acromegaly is commonly treated through surgical procedures. Patients who refuse this line of treatment are treated with somatostatin receptor ligands, growth hormone receptor antagonists, dopaminergic agonists, or radiotherapy.
Filed under: adrenal, Cushing's, pituitary, Rare Diseases, symptoms, Treatments | Tagged: acne, Acromegaly, Cushing Syndrome, hypertension, ketoconazole, mitotane, muscle weakness, Osilodrostat, paraganglioma, pheochromocytoma, primary aldosteronism, purple stretch marks, Weight gain | Leave a comment »





 View Full Size
View Full Size View Full Size
View Full Size View Full Size
View Full Size