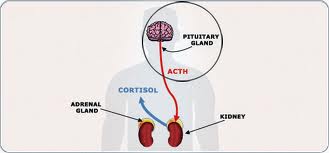
Patients with adrenal incidentalomas and mild hypercortisolism have an increased risk for cardiovascular events and mortality. This risk was evident even when clinical signs of overt hypercortisolism were not present, according to data published in The Lancet Diabetes & Endocrinology.
“Our findings are important because they add to the previously scant information about adrenal incidentalomas, which will be of use to doctors who are seeing an increasing number of patients with these masses,” Renato Pasquali, MD, of the S. Orsola-Malpighi Hospital in Bologna, Italy, said in a press release.
The retrospective study by Pasquali and colleagues assessed the adrenal incidentalomas of 198 outpatients treated every 18 to 30 months, with a mean follow-up of 7.5 years. At the time of follow-up, 114 patients demonstrated stable non-secreting adrenal incidentalomas (<50 nmol/L), 61 had either a stable intermediate phenotype (50 nmol/L-138 nmol/L) or subclinical Cushing’s syndrome (>138 nmol/L), and 23 patients had worsening pattern of secretion.
The incidence of CV events appeared higher in patients with a stable intermediate phenotype or subclinical Cushing’s syndrome (6.7% vs. 16.7%; P=.04) and in those with worsened secreting patterns (6.7% vs. 28.4%; P=.02) compared with patients with stable non-secreting adrenal incidentalomas, according to data.
In addition, CV events were independently related to changes in cortisol concentrations after the 1-mg dexamethasone suppression test (DST; HR=1.13; 95% CI, 1.05-1.21) from baseline to follow-up.
Patients with stable intermediate phenotype adrenal incidentalomas (57%) or subclinical Cushing’s syndrome (91.2%) tended to have lower survival rates for all-cause mortality (P=.005), researchers wrote. The main risk factors for all-cause mortality were age (HR=1.06; 95% CI, 1.01-1.12) and mean concentrations of cortisol after DST (HR=1.1; 95% CI, 1.01-1.19).
The unadjusted survival for CV-related mortality was lower in patients with either a stable intermediate phenotype (97.5%) or subclinical Cushing’s syndrome (78.4%; P=.02) vs. those with stable non-secreting adrenal incidentalomas (97.5%), and patients with worsened secreting patterns (60%; P=.01).
In an accompanying comment, Rosario Pivonello, MD, PhD, Maria Cristina De Martino, PhD, and Annamaria Colao, MD, PhD, of the Federico II University of Naples, Italy, wrote that the study supports the importance of long-term hormonal follow-up for clinical management of patients with adrenal incidentalomas.
“Furthermore, clinical monitoring of cardiometabolic risks seems to be important in these patients, particularly in those with subclinical Cushing’s syndrome and intermediate phenotype adrenal incidentalomas, for whom medical or surgical intervention could be needed,” they wrote.
They suggest long-term prospective studies to determine the frequency of new CV events and mortality in this patient population.
For more information:
Di Dalmazi G. Lancet Diabetes Endocrinol. 2014;doi:10.1016/S2213-8587(13)70211-0.
Pivonello R. Lancet Diabetes Endocrinol. 2014;doi:10.1016/S2213-8587(13)70190-6.
Disclosure: The researchers report no relevant financial disclosures.
This article is from http://www.healio.com/endocrinology/adrenal/news/online/%7B85f94352-9529-4cb7-9532-9c4518f77d80%7D/cv-risk-elevated-in-patients-with-adrenal-incidentalomas-mild-hypercortisolism
Filed under: adrenal, Cushing's | Tagged: adrenal, cardiovascular, Cushing's Syndrome, dexamethasone suppression test, hypercortisolism, Incidentaloma | Leave a comment »